The American Gastroenterological Association (AGA) published a research report in the April 2020 issue of Gastroenterology. The report titled – “Causes of Post-Colonoscopy Colorectal Cancer (PCCRCs) Based on the World Endoscopy Organization (WEO) System of Analysis” found several key factors that could improve and prevent up to 89% of PPCRCs.
What is PCCRC?
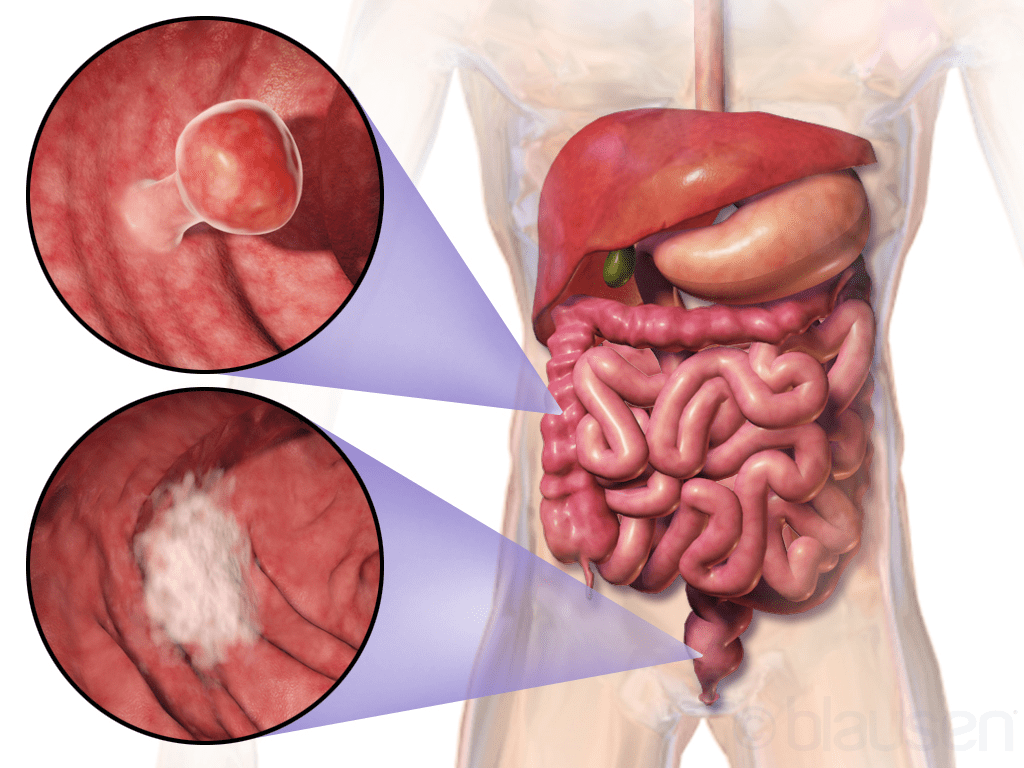
PCCRC is colorectal cancer (CRC) diagnosed after a colonoscopy in which no cancer was found. PCCRC-3y is an interval for PCCRC, indicating colorectal cancer detected after 6 months to 3 years of a colonoscopy session. AGA has a target rate of 2% for the PCCRC-3y interval and below are several improvements to be made to achieve the target.
5 Major Factors
The AGA research report suggested a list of factors associated with PCCRC, this article will focus on 5 of the key factors.
1. Inadequate bowel preparation
Bowel preparation is extremely important as it allows doctors to see any abnormalities, such as colon polyps during the procedure. Yet, 19.0% of investigated cases in the research have reported inadequate bowel preparation. In 45% of those cases, the clinicians did not repeat the procedure, arrange alternative investigations, or make an explicit statement to further investigate, which AGA strongly advised and recommended colonoscopists to do so.
2. Retroflex in the rectum
Retroflexion refers to making a U-turn with the bending section of the colonoscope. The AGA report suggested that rectal retroflexion should be a key performance metric, and indicator for adequate visualization of the rectum. In addition, it is a significant shortcoming to not perform such a procedure, however, retroflexion was documented in only 16% of 100 cases.
3. Inadequate photo-documentation
Accurate and adequate image documentation is an essential part of GI endoscopic reporting, but only 36.3% of studied colonoscopies had adequate photographic evidence of completion. This reflects a lack of appreciation of the importance of cecal photographs (photos of the cecum, which is a pouch that forms the first part of the large intestine). With approximately 20% of colorectal tumors develop in the cecum, adequate photo-documentation of the cecum should always be practiced as it is also a key performance metric in all colonoscopy guidelines.
4. Chromoendoscopy not performed
Chromoendoscopy (CE) is an image-enhanced colonoscopy techniques that involve spraying dye to colonic mucosa. The dye improves the detection of abnormal cell growth in inflammatory bowel disease (IBD) surveillance. In the AGA research report, CE was used in just 11.1% of colonoscopies for PCCRCs developing in patients with IBD. In cases where CE is not possible, there is no documentation explaining why dye spray was not used. Proper documentation and further reorganization can help overcome shortcomings in IBD surveillance.
5. Long wait time
In the AGA study, more than 16% of the cases were affected by administrative delays in surveillance or planned therapeutic procedures. Patients scheduled for surveillance procedures are a lower priority than symptomatic or screened patients and often wait beyond their due date, but for a small number, a delay becomes important.
